Website: tamingthezebra.org
Mailing List: https://www.tamingthezebra.org/join-the-email-list
Excerpt from: Taming the Zebra – It’s Much More than Hypermobility: The Definitive Physical Therapy Guide to Managing HSD/EDS, Volume 1 Systemic Issues and General Approach
(Due out Winter of 2023)
CHAPTER 2
Understanding Connective Tissue
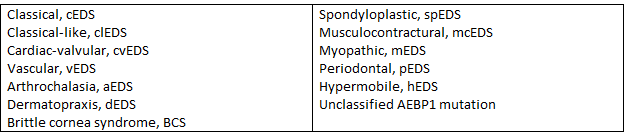
The Ehlers-Danlos Syndromes (EDS) are described as a group of heritable heterogenous connective tissue disorders, meaning different genetic variations are present with different classifications of EDS. EDS is not simply a diagnosis of joint hypermobility, but a reference to a connective tissue disorder throughout the body, involving many different systems. Presentation with each patient will be determined by the type of genetic variation identified along with genetic expression, which is further discussed below.
The human body is made up of nervous, muscular, epithelial (skin), and connective tissue. Connective tissue can be found in the nervous and muscular tissue and adjacent to the epithelial tissue. Connective tissue plays many different roles for us within our bodies (Figure 2.1). It helps package and compartmentalize areas of the body by providing support or protection. It can bind and separate organs or other tissues. Connective tissue also plays a role in protection, defense, and repair. It aids in scar tissue formation, inflammation, and defense against invading bacteria or other substances through some of its molecular components. It acts as insulation, storing energy as adipose tissue (fat). It also assists in transportation throughout the body. Blood is a connective tissue that delivers oxygen and nutrients throughout the body. Blood is considered a connective tissue because it consists of blood cells surrounded by a fluid matrix called blood plasma. Fascia is a connective tissue creating a continuous system throughout the body, becoming a means of directing and transferring mechanical forces within the body. If, however, the connective tissue is dysfunctional, this can lead to the transfer of inefficient forces and lead to imbalances and/or restrictions. It is thought that the connective tissue is the medium for acupuncture treatment and explains how needles affect organs from afar. Myofascial release experts purport that memory can be stored in the guarding patterns of the tissue, explaining some chronic, non-responsive fascial dysfunction. Connective tissue is complex and expansive within the human body.
| Roles of Connective Tissues Throughout the Body |
| Packaging and Compartmentalizing Protection, Defense, and Repair Insulation Transfer of Mechanical Forces Throughout the Body |
| Figure 2.1 Connective tissues assists with many different functions and roles within the human body. A connective tissue disorder can cause issues in any of these roles listed. |
Connective tissue is the most abundant tissue in our body, found just about everywhere. It is found in fibrous tissues, fat, cartilage, bone, bone marrow, tendons, the wall of the gastrointestinal system, skin, and blood vessel walls. It also encloses the brain and spinal column. Connective tissue is made up of many different components, primarily elastin, collagen fibers, ground substance (gelatinous material that fills the spaces between fibers and cells), and immune cells. Those collagen fibers along with proteoglycans (protein) and glycosaminoglycans (polysaccharide compound) together make up the extracellular matrix along with other compounds. The distribution and ratio of each of these in a particular make-up of connective tissue will determine what the connective tissue looks like (i.e. fibrous versus ligamentous). The function of the connective tissue is determined by the protein composition of the extracellular matrix (ECM). The immune cells reside in the extracellular matrix.
Figure 2.2 Connective tissue within the human body makes up cartilage, tendon, bone, adipose tissue, and ligaments. Connective tissue surrounds the blood vessel walls, muscles, and nerves, also influencing these systems as well.