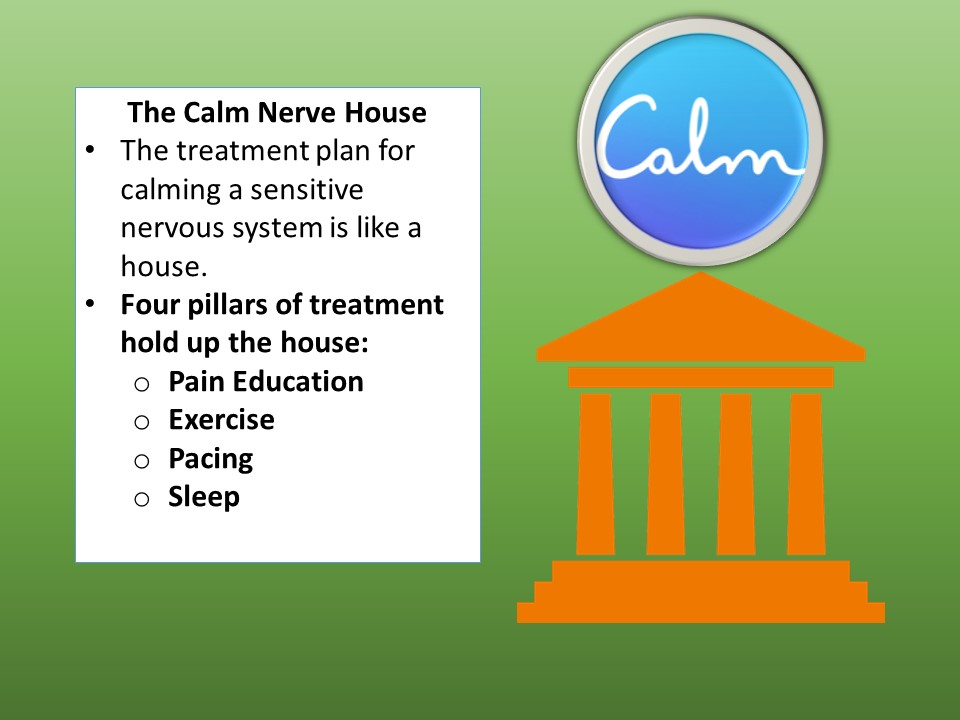
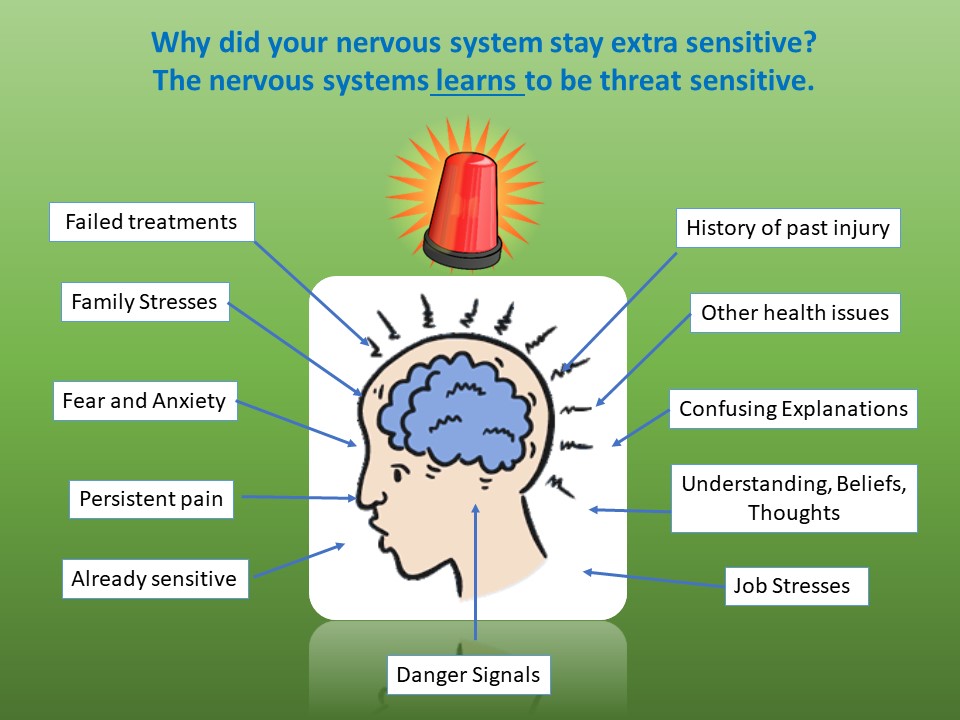
Hello, Zeborah Dazzle, PT, WWF here — spokes-zebra and patient educator for Good Health Physical Therapy. We have been talking about pain over the last four posts, and specifically how, in some situations, the nervous system can become sensitized to keep pain levels stirred up. In these instances, the nervous system itself can be as much or more of a cause of the chronic pain than any tissue damage. When the spinal cord and brain become sensitized, this is called central sensitization. So, our question is how to calm the sensitized nervous system? The model we use is the Calm Nerve House and the basic pillars supporting the house are Pain Education, Sleep, Exercise and Pacing. However, inside the Calm Nerve House there are a number of other self-care techniques which can be calming. Here are a few:
MASSAGE
There are many kinds of massage therapy. It is wisest to seek out a licensed (which means trained) massage therapist. As a general rule, massage that hurts is NOT helpful for a sensitized nervous system. Firm but gentle massage though, a session aimed at relaxing you can be very soothing.
SMOKING CESSATION
There are several ways in which smoking can increase pain levels. First, smoking floods the lungs and the blood stream with nicotine which is a stimulant. This leads to a nervous system even more on edge. Additionally, besides the damage done directly to lungs which most people are aware of, smoking floods the lungs and blood with carbon monoxide. This compound attaches to the red blood cells whose job is to carry oxygen to every part of your body. So, besides the risk of cancer and lung disease, smoking has the negative effect of depriving vital oxygen to bone, muscle, connective tissue and nerves.
DIET
While we will not attempt to give specific rules about diet here, it is very wise to remember that the health of the nervous system depends on good nutrition. There have been some powerful studies done over the last few years looking at what the best diet is for humans, and a good general rule is the adage coined by popular author John Robbins: Eat food, not too much, mostly plants.
Another tip is to decrease caffeine consumption. Caffeine is a nervous system stimulant and will tend to turn up the volume on a sensitized nervous system.
MEDITATION
In 1975, Herbert Benson MD published “The Relaxation Response.” Dr. Benson showed that relaxation techniques such as meditation have immense physical benefits, from lowered blood pressure to a reduction in heart disease. In his book “Full Catastrophe Living” Dr. Jon Kabat-Zin describes positive results achieved with chronic pain sufferers employing mediation and mindful techniques. Virtually every religious tradition teaches a meditation technique as a form of prayer, but meditation does not need to be a religious practice. (And you don’t have to sit cross legged.)
SELF TALK (THOUGHTS AND BELIEFS)
Our thoughts, and what we choose to believe, have a strong effect on our nervous system and can either increase or decrease stress leading to increased or decreased sensitization. One of the most single toxic beliefs you can take on is: “This pain will never get better.” A trick is to say “cancel” whenever you think this or any other negative declaration. Then work to replace this thought with a positive one such as: “This will pass.”, “I can handle this.”, or “I am getting a little bit better each day.”. A counselor or trusted spiritual advisor is often an extremely important part of your care team and can help with beliefs and self-talk.
HUMOR
Have you ever noticed that you cannot simultaneously feel depressed or anxious or overwhelmed by pain and having a good belly laugh? This is because laughter floods the brain with natural pain killing chemicals (neurotransmitters). So, we recommend that you make funny movies, people who make you laugh, funny stories, jokes and stand-up comics a regular habit. Humor helps, and that’s no joke.
In coming posts, we will look at other topics including exercise and hypermobility spectrum disorder/ hypermobile Ehlers-Danlos Syndrome.
I would like to thank Dr. Mark Melecki PT for his assistance with this series which relied heavily on materials he compiled for his physical therapy doctoral project.
Until next post, Cheers!
Zebbie