Hello,
My name is Zeborah Dazzle, PT, WWF, and I am the new spokes zebra and a patient educator for
Good Health Physical Therapy. I am posting some educational pices in between seeing patients, and we
have been discussing pain, especially chronic pain, which is something very familiar to those of us with
EDS and hypermobility.
I finished my last post by describing how the nervous system can become overly sensitized so that the
pain perception being created is no longer in proportion to the injury in the body. As I described, the
nervous system with the brain at the top, is the sensory and control system of the body. Pain is a perception that is the brain’s estimate that the body is being harmed. And it does not always make the
estimate accurately.
When an area of the body has been injured repeatedly, the local nerves can become overly sensitized
and send too many signals to the brain – out of proportion to the injury. This is called peripheral
sensitization. Similarly, there are connector nerve cells in the spinal cord that can get overly sensitized
and allow too many signals to pass to the brain. And finally, the brain is a learning organ and will make
it’s estimate of potential injury based on past experiences and current stresses. Sensitization of the
spinal cord and/ or the brain is called central sensitization. Practically, this means that the nervous
system itself may be as much or more of a problem than any injury to the body such as sprains, strains
or hypermobile joints.
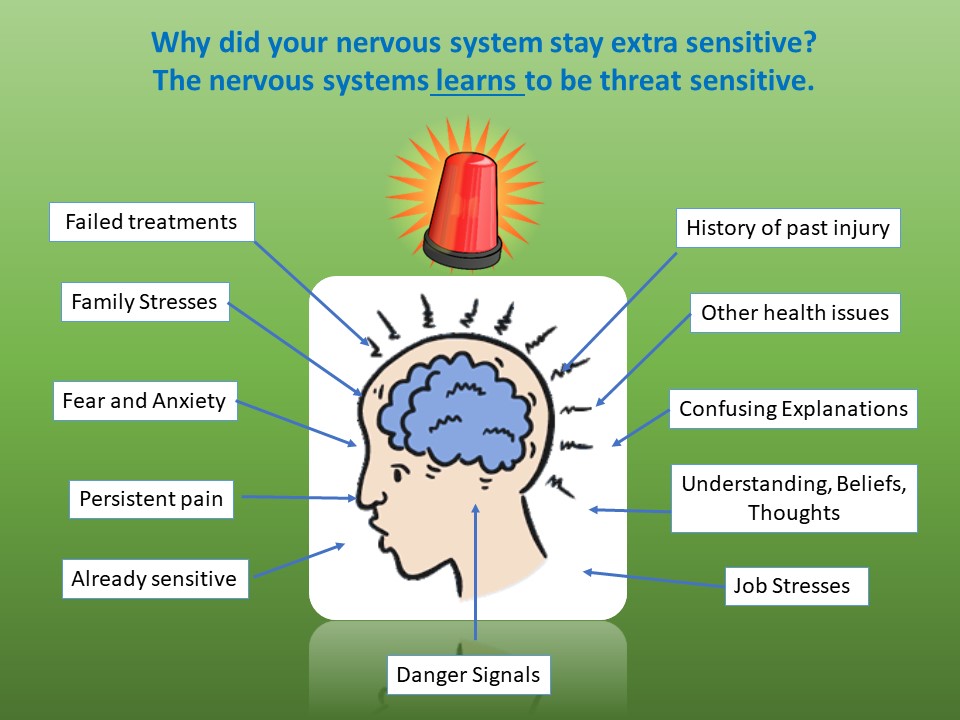
When nerve danger signals hit the brain, they are interpreted by a number of areas of the brain working
together. If the person has a past history of being injured or of physical or emotional stressors, the brain
may over interpret the signals and create too much pain or pain over too large an area. (See the
illustration of different factors that can cause the brain to overestimate.)
How do we get the nervous system to calm down and stop blaring its warning messages (pain)?
One avenue to calm the nervous system can be medication. All medications have their pros and cons, so
we believe that it is very important that you work with your primary care provider to find the right
strategy of medications to use – even if you are just using over-the-counter medications. Now, as you
probably know, we physical therapists do not prescribe drugs though and we have some other
strategies.
It can be useful to look at non-drug approaches to calming the nervous system as being like a house: the
Calm Nerve House. All solid houses have sturdy pillars which hold them up and so does the Calm Nerve
house; while there are many healing approaches in the Calm Nerve House, the pillars are:
Pain Education – understand your pain and how it works. Knowledge gives power. (This is what
I am working toward with these posts.)
Sleep – a fatigued nervous system is a nervous system on edge
Exercise – “motion is lotion”
Pacing – too much lotion creates commotion
We will talk more in-depth about each of the pillars and some of the content of the Calm Nerve House in
coming posts.
Until next time – Cheers!, Zebbie