4.24.2023
POTS 3: Exercise
For the past two blog posts, we have been talking about Postural Orthostatic Tachycardia Syndrome (POTS). This is an imbalance of the involuntary nervous system which may occur in a number of different health situations, such as post COVID, but is common especially for patients with hypermobility spectrum disorder (HSD) and hypermobile Ehlers-Danlos Syndrome (hEDS).
POTS is the more severe end of a spectrum of symptoms all due to imbalances of the involuntary nervous system (the autonomic nervous system) called dysautonomia. The main symptoms of POTS are a racing heart that happens when the person stands up and feeling lightheaded, dizzy or just ill.
There are conservative and medication treatments for all of these types of POTS, and these are summarized in the last blog post (POTS 2). But one conservative treatment that research is showing to be beneficial for all of the types of POTS is exercise. {6}
Studies of patients with POTS have shown that cardiac atrophy, or weak heart, is a key component of the pathology. {4} Exercise improves but does not necessarily normalize heart function. {4} Exercise study participants lowered their resting heart rate and improved pain, sleep, overall energy, work capacity and several other indicators of quality of life. {3} More than one study has shown that exercise can help patients move fully into remission from POTS with 47-70% of participants going into remission in two studies.{3} One study found that exercise was better than the drug propranolol in helping the heart improve function. {1}
What Kind of Exercise?
Now we know from experience of working with patients that exercise is not always an easy sell for someone who already feels bad day to day. But we also know the incredible strength and courage of our patients. So, take a deep breath, and let’s ease in to talking about this.
Overall, we are talking about both aerobic conditioning exercises such as swimming, rowing, cycling, elliptical trainer, treadmill walking, or running. Additionally, in many cases resistance training, such as therapy bands, weight lifting or Pilates, is a very important part of the program. As we have talked about previously, POTS is a syndrome which represents the more severe end of dysautonomia, but even in this more sever end there is a spectrum of severity and so the exercise program itself must be tailored to fit.
Aerobic Exercise {2,3, 4, 5}
What Does it Mean: Exercise Tailored to Fit?
There are a number of variables that are considered in designing a plan: intensity, frequency, and duration are the most common.
Intensity
Before deciding the intensity of the exercise, how hard it is, the severity of the POTS case must be considered and the type of exercises chosen. For patients who are having severe symptoms, all exercises are started lying down. The more severe the case, the closer to lying flat the program is started. There are types of exercise bikes that can be done by someone lying supine. Swimming can also be done with the body in the horizontal position. After a number of months, these exercisers can progress to more upright exercises such as a recumbent bike or a rowing machine. And after additional time, upright exercises can be added such as an upright bike, elliptical trainer, walking, and running.
For each individual exercise the cardiac intensity, how hard the heart is working, can be judged one of three ways: heart rate, rating of perceived exertion and, sometimes simply, a “talk test”.
Judging Cardiac Intensity
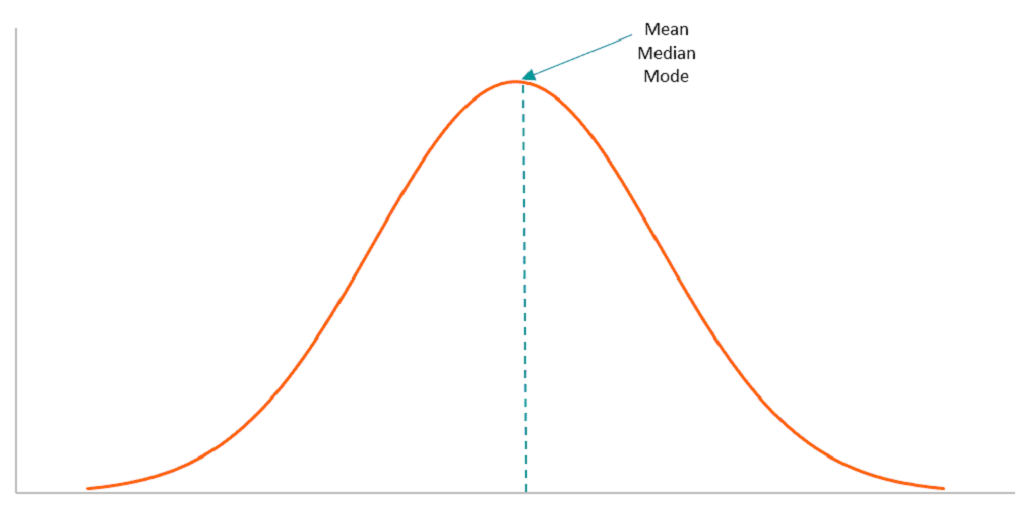
For each person there is a maximum number of heart beats per minute which their heart is capable off, called heart rate max (HR Max). The number that is normally used as a reference in textbooks is 220 beats per minute. But this number gets lower with age. So, heart HR Max is estimated with the a formula: (220-persons age) +/- 5 beats per minute.
For example, a 30-year-old would have a theoretical HR Max of (220-30) = 190 +/- 5 beats. For exercise, a percentage of this is taken to determine how hard the person is working, usually between 60-85% of HR Max.
Another good indicator of intensity is to ask the exerciser to rate how hard they are working. This is called “rating of perceived exertion” (RPE) and while there are some different scales for this, a common one is the “Borg Scale” based on a number rating from 6-20.
| RPE | How hard are you working? |
| 6 | No exertion; sitting, resting |
| 7 | Extremely light |
| 8 | |
| 9 | Very light |
| 10 | |
| 11 | Light |
| 12 | |
| 13 | Somewhat Hard |
| 14 | |
| 15 | Hard |
| 16 | |
| 17 | Very Hard |
| 18 | |
| 19 | Extremely hard |
| 20 | Maximal exertion |
In Germany, for many years, there have been hiking clubs where they keep exercise at a moderate level by singing, or at least talking as they hike. If a person is having trouble singing while they exercise, they are working too hard. This is one kind of a “talk test”.
Workout Intensity Levels
In the exercise programs for POTS there are three levels of intensity for workouts whether the exerciser is supine, sitting or upright: Base Pace, Maximal Steady State and Recovery.
Base Pace. This is the basic level of exercise and is normally preceded and followed with a 5 minute warm-up and a 5 minute cool down. Base pace intensity exercise just starts to make it challenging to talk, perceived exertion is rated between 13-15 (between somewhat hard and hard), and results in a heart rate around around 75% of HR Max.
Maximal Steady State. This is intense exercise usually undertaken later in the workout program when fitness levels are improving. During this level of intensity, the patient will not easily be able to talk or sing, rates their exertion between 16-18 (very hard) and results in heart rate around 85% of HR Max.
Recovery. Recovery workouts are done on days after a Maximal Steady State workout. At this level of intensity, the talk test is easily passed, rating of perceived exertion is between 6-12 (fairly easy) and results in heart rate around 60-65% HR Max.
Frequency and Duration
How often (frequency) the person exercises and how long (duration) — meaning both the total program length and the daily workout length — will all vary depending on where the person is on the spectrum of POTS symptoms. Again, patients at the severe end of the spectrum will start all exercises with their body horizontal, such as lying down or swimming.
The Children’s Hospital of Philadelphia plan {5} describes a 5-month program. Exercisers will progress to more upright forms of workout at the end of the first or second month depending on their body. The researchers at Texas Health {2} describe a 3-month program. Exercisers with a mild or intermediate level of POTS may start all exercises sitting or sometimes even standing.
Initially, exercisers will participate in 3-4, 25-30 minute workouts per week at a Base Pace. Progression to the next level of workout may be started at the end of the first to third months of the program or even longer depending on how the person’s body responds. In the next harder level, exercisers will progress to one and then two Maximal Steady State workouts per week. This level of workout is always followed by a Recovery workout. By the end of program, exercisers will be performing 5-6 workouts per week of 45-60 minutes each.
As with all exercise, to attain the desired response from the body, persistence and consistency are needed. So, if more than two workouts are missed in a week, that week is repeated. If two weeks or more are missed, the entire program is restarted.
Resistance Training {2, 3, 4, 5}
Especially in cases where hypermobility is involved, resistance training is another part of the exercise program. Resistance training can and often does mean weight lifting, but may also include resistance bands and the resistance of the exercisers own body weight. Pilates exercise is a good example of this.
Exercisers are well advised to be mentally ready to be sore. This means sore muscles but should not include flaring up sensitive areas. To avoid this starting at the right level, which may be very light for some, and progressing gradually are important.
Especially for those with more severe POTS will begin lying down or sitting. Those with mild or intermediate symptoms may begin standing but should sit immediately after exercise. Workouts begin once per week for 15-20 minutes and gradually increase to twice per week building to 30-40 minute sessions. In selecting exercises, special emphasis is placed on lower extremity and core strengthening. It is important to take at least two days off between resistance workouts – this is the time when the body adapts and grows stronger.
As you can tell from reading all of this, the direction of a skilled therapist will be very important for this kind of treatment. Even though it can be challenging to find a therapist who is knowledgeable about hypermobility, dysautonomia and POTS, seeking one out can be very worthwhile.
We are still thinking about what to write about next in this blog series. Future topics may include mindfulness, digestive issues in HSD and hEDS and others.
Until then, cheers!
Zebbie
Zeborah Dazzle, PT, WWF
Spokes-Zebra and Patient Educator for Good Health Physical Therapy and Wellness.
Thanks to Dr. Mark Melecki, PT for his assistance in preparing this blog. (It is very challenging to type with hooves rather than fingers. Thanks Mark.)
References:
- Fu, Q and Levine, BD, Exercise and Non-Pharmacological Treatment of POTS, Auton Neurosci. 2018, December; 215:20-27.
- Fu, Q, et. al., Exercise Training Versus Propranolol in the Treatment of the Postural Orthostatic Tachycardia Syndrome, Hypertension Volume 58(2), August 2011; pages 167-175
- Adger, K and Lynch, H., Exercise in the Management of Orthostatic Tachycardia Syndrome, Journal of Kinesiology and Wellness, 9(2), July 2020, pages 28-37
- Shibata, S., et. al., Short-term Exercise Training Improves Cardiovascular Response to Exercise in the Postural Orthostatic Tachycardia Syndrome, J. Physiol 590.15 (2012) pages 3495-3505
- Children’s Hospital of Philadelphia, Instructions for POTS Exercise Program, unpublished paper.
- Zadourian, A., et. al., Postural Orthopedic Tachycardia Syndrome: Prevalence, Pathophysiology, and Management. Drugs (2018) 78:983-994
- https://www.texashealth.org/ieem/Patient-Care/Syncope-and-Autonomic-Dysfunction-Clinic