2022.11.10
Basics
Hello, Zeborah Dazzle, PT, WWF here. I am the spokes-zebra and patient educator for Good Health Physical Therapy and Wellness.
As some of you know, while I am a physical therapist who treats all kinds of problems, including all kinds of bone and muscle problems, my special interest is Ehlers-Danlos Syndrome (EDS) and Hypermobility Spectrum Disorder (HSD). Sometimes it is wise to pause and go back to basics. That is what I will focus on with this and the next post.
What is Ehlers-Danlos Syndrome?
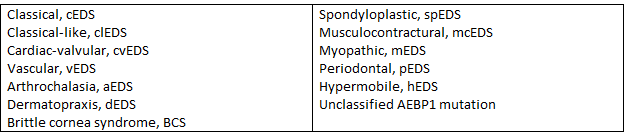
Ehlers-Danlos Syndrome (EDS) is a group of inherited connective tissue disorders. At present, there are thirteen variations of the disease. All involve fragility of one or more of the 28 types of collagen which is the major part of connective tissue.
Connective tissue supports, protects and holds the tissues of our bodies together. It includes tendons, ligaments, blood and the support structures for arteries, veins and muscles as well as internal organs. It is very important in the body, and it is EVERYWHERE. A colleague of mine likes to tell patient’s that if he was an evil wizard and waved a wand that took away all other cell types in your body other than connective tissue, there would still be a perfect three dimensional you remaining. (You would be dead though and we could probably shine a flashlight through you – bad wizard.)
Among the thirteen different types of EDS are types which predominantly affect different parts of the body especially the heart, the blood vessels, the eyes, skin, gums and bones/ joints. Here is a list of the names of the thirteen.
How Common is Ehlers-Danlos Syndrome?
The different EDS types range from uncommon to very rare in the general population. The single most common type of EDS is Hypermobile Ehlers-Danlos Syndrome (hEDS). The prevalence of this condition is estimated by the Ehlers-Danlos Society as 1/3500 to 1/5000 people. That means that out of the 332,218,200 people in the US there may be 94, 919 (0.02%) of the population with hEDS. The other kinds of EDS are much less common ranging from 1/40,000 (about 8,305 people, .003%) to 1/1 million people (about 332 people). I believe these estimates are low due to under diagnosing.
How is Ehlers Danlos Diagnosed?
Of the thirteen different types, there are genetic tests for all but the most common, hEDS. As a result, the diagnosis of hEDS is performed by evaluating a patient through three criteria levels. In the first level, hypermobility, or excessive stretch/ flexy/ bendy-ness is screened for. In the second level, physical characteristics commonly associated with hEDS are screened including some physical characteristics, skin texture and stretchiness and common medical history indicators. In the last criteria level, a physician must rule out other conditions which can mimic the symptoms of hEDS. It is common for patients to come to see me and want me to diagnose hEDS. Physical therapists are trained to evaluate and diagnose movement disorders and to correlate these with medical problems which sometimes means screening for problems. So, as a PT, I can diagnose hypermobility but only screen for hEDS. I cannot not diagnose it formally because I cannot rule out other conditions. Patients who are hypermobile but do not fit the diagnostic criteria of hEDS are diagnosed with hypermobility spectrum disorder (HSD). More on this in a later post.
Why Do People with Ehlers-Danlos Syndrome Call Themselves “Zebras”?
In the next post, we will go into more detail about the kinds of problems that EDS can cause, but for now let me simply say that they are multiple and often appear to be unrelated – joint pain in many areas of the body, bruising, strains, sprains, subluxations or dislocations, gut problems, dizziness and many more. For this reason, people with EDS do not fit in to a quick common pattern for diagnosis.
When medical students are trained, they spend a great deal of time learning about different conditions and the symptoms they can create. Because common symptoms can so often be caused by different underlying conditions, this makes diagnosis hard. Almost all medical students are taught this aphorism: If you hear hoofbeats, think horses, not zebras.
This is a good thing overall. Afterall, if Mrs. Smith comes in to see the doctor complaining of a sore throat, the most probable cause is something common. Perhaps she was shouting at a football game or perhaps she has a cold. Throat cancer is much farther down the list.
The problem for EDS patients though is that we are actually zebras (or in my case a zebra-zebra). Beginning medical training in anatomy is changing in medical school these days, but traditionally anatomy was taught by cadaver dissection. During this process, connective tissue is commonly the stuff put in the container under the table while the student is looking for another structure like a nerve or a blood vessel or an organ or a muscle. Is it any surprise, that a connective tissue disorder is often not on the doctors mental list of potential diagnoses? I am hopeful that this is changing, but in the meanwhile, it is up to all of us with HSD or EDS to educate ourselves so we can partner with our providers in the most positive way.
In the next post, we will look more closely at hypermobility spectrum disorder and the symptoms that HSD and EDS can create as well as an overview of treatment principles.
Until then, Cheers! Zebbie
Thanks to Dr. Mark Melecki, PT for his assistance in writing this blog. (It is very challenging to type with hooves rather than fingers. Thanks Mark.)