9/6/22 Pain 3
Hello, Zeborah Dazzle, PT, WWF here — spokes-zebra and patient educator for Good Health Physical
Therapy. We have been talking about pain over the last two posts, and specifically how, in some
situations, the nervous system can become sensitized to keep pain levels stirred up. In these instances,
the nervous system itself can be as much or more of a cause of the chronic pain than any tissue damage.
When the spinal cord and brain become sensitized, this is called central sensitization. So our question is
how to calm those sensitized nervous system?
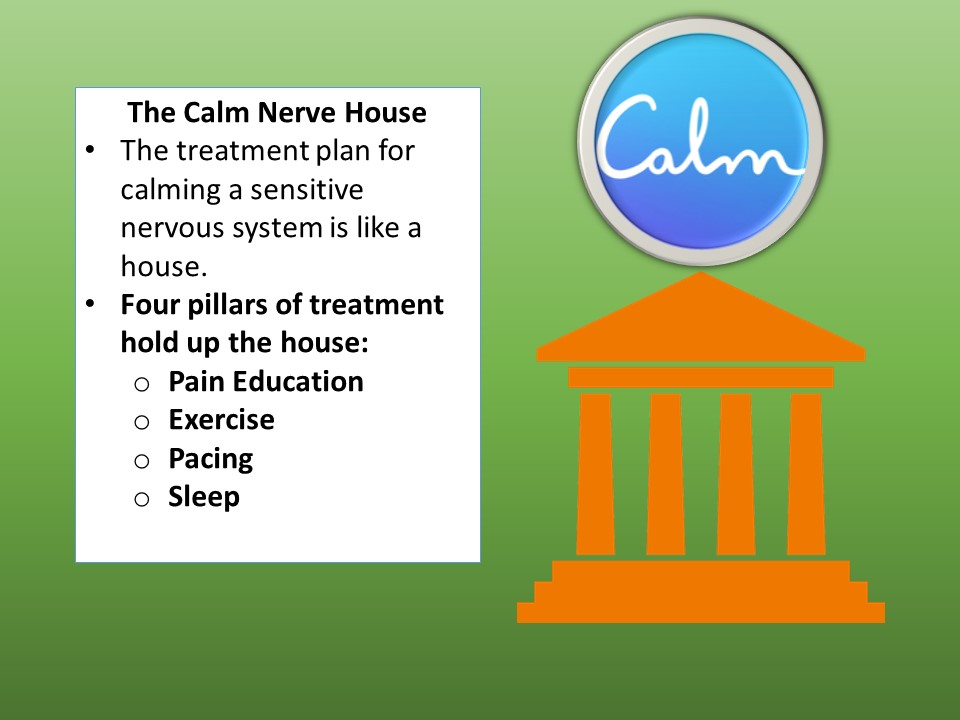
The best results in therapy often happen when multiple approaches are used in a coordinated plan. The
model we use is the Calm Nerve House and the basic pillars of the house are Pain Education, Sleep,
Exercise and Pacing. Today, let’s talk more about pain education and sleep.
PAIN EDUCATION
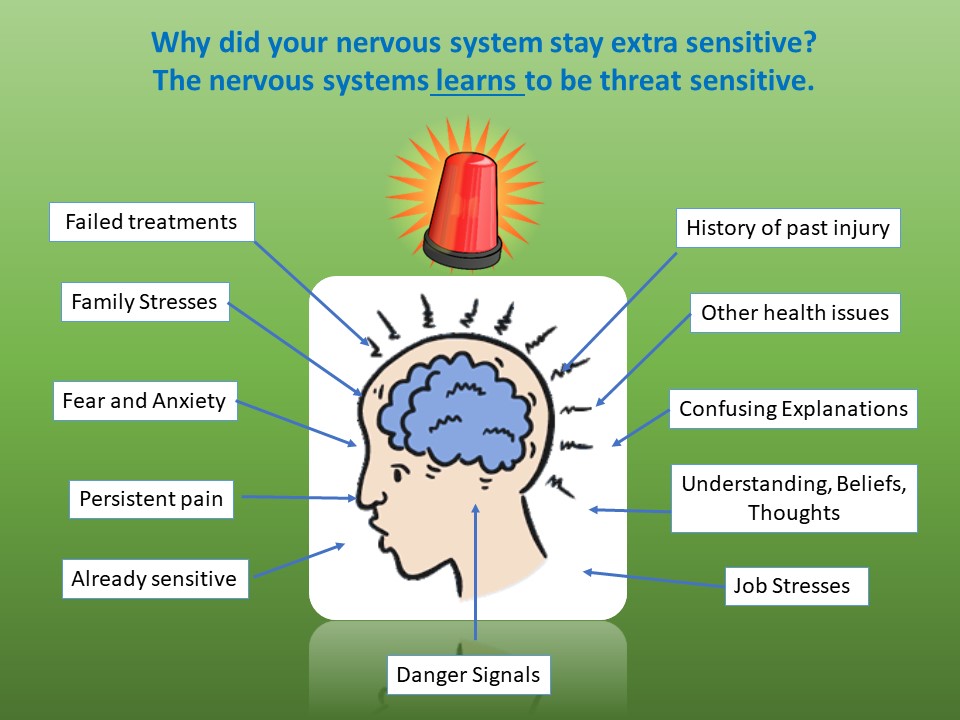
Recent studies have shown that pain education (just the type of thing you are getting in these posts) can
have a positive effect on pain. When patients understand what is happening in their bodies, this helps to
lower fear levels which in turn helps to calm the brain. Additionally, understanding the different factors
which can add together in the brain (See diagram) to sensitize the brain, can be a big help for patients
on their healing journey. For example, knowing that old emotional traumas can teach the brain to be
extra alert for potential injuries, can help guide a patient toward getting help with that trauma. And
knowledge of the other kinds of stresses which sensitize the nervous system can lead the patient to
problem solves ways to lower those stresses. Knowledge is power, especially when we use that
knowledge to guide our decisions.
SLEEP
A fatigued nervous system is a sensitive nervous system, so sleep is crucial to pain control. There is no
one perfect piece of advice to help with sleep, but below is a general list of tips.
Lifestyle
Get regular exercise each day, preferably in the morning. There is good evidence that regular
exercise improves restful sleep and overall health. This includes stretching and aerobic exercise. Try
to limit exercise 3 hours before bedtime.
· Get plenty of sunlight outdoors, particularly later in the afternoon.
· Use the evening hours for settling down. Avoid challenging or stimulating activities and avoid bright
lights in the evening 2-3 hrs. before bedtime.
· Try to avoid naps during the day.
· Pick a regular bedtime and wakeup time and stick to them throughout the week.
· Avoid all bright screens including phones, tablets, TVs, or other tech devices 1 hour before going to
sleep.
· Once you are in bed, relax from head to toe and guide your mind to pleasant thoughts.
· Don’t command yourself to go to sleep or “clock watch”. This only makes the mind and body more
alert.
· If you lie in bed awake for more than 20-30 minutes, get up and go to a different room to do a quiet
activity. Return to bed when you feel sleepy. Do this as many times during the night as needed.
Food and Drink
Although small snacks can help you get to sleep, don’t eat a large meal about 2 hours prior to
sleeping.
Limit how much you drink at night to reduce your need to get up to urinate, but don’t go to bed
thirsty.
Stop all caffeine consumption no later than 6 hours before you are planning on going to bed.
Avoid all forms of nicotine prior to sleeping including cigarettes, chewing tobacco, and vaping.
Avoid drinking alcohol before bed.
Environment
Keep your bedroom quiet, dark, and cool. Try using a sleep mask and/or earplugs to help you sleep.
Run a fan or other steady “white noise” during the night if noises wake you up.
Reserve the bed for sleeping, sickness or sex only. Do your reading or TV watching in another room.
Keep your hands and feet warm. If needed, wear warm socks and/or gloves to bed.
Wear loose-fitting nightclothes. The more comfortable you are, the better you will sleep.
Try not to sleep with disruptive bed partners such as your children, pets, or spouses.
Until next post – Cheers!
Zebbie